
Ocular Surface Diseases
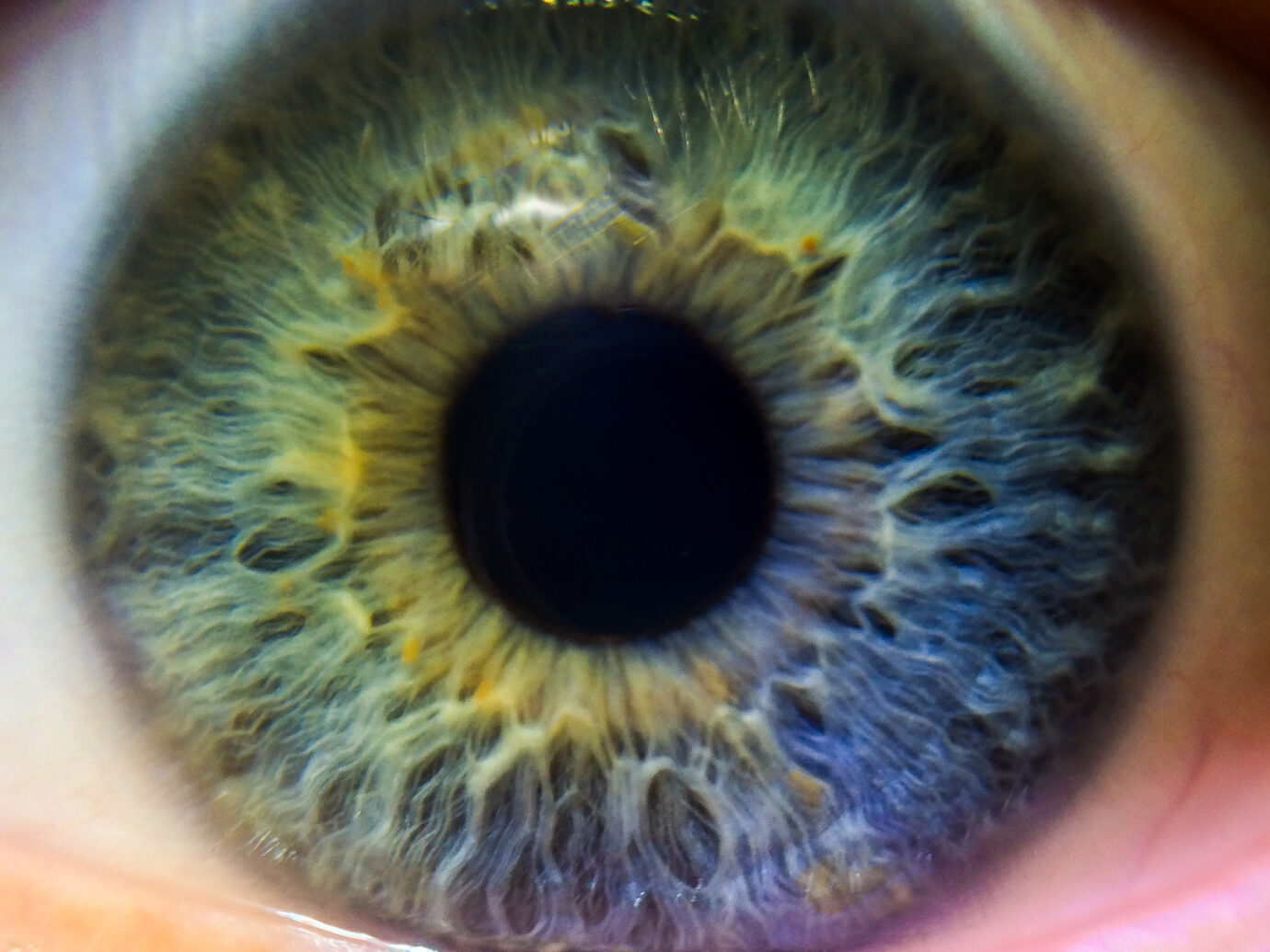
The ocular surface is essential for vision and provides the main refractive surface that bends light as it enters the eye allowing clear sight. It is comprised of the outer front layers of the eye and the structures surrounding it which include the cornea, conjunctiva, lacrimal glands, meibomian glands, and tear film.1 Ocular surface diseases (OSDs) are a family of disorders that affect these structures and represent a leading cause of patient visits to the eye doctor.2,3 Dry eye disease and allergic conjunctivitis are the most common OSDs, with the potential to severely impact patients’ quality of life.4
About Chronic Dry Eye and Episodic Dry Eye Flares
Dry Eye Disease (DED) is a disease of the ocular surface characterized by tear film instability and is usually accompanied by ocular surface inflammation and damage.5 More than an estimated 16 million adults have been diagnosed with DED in the United States and with an estimated global prevalence between 5 to 50%, it is one of the most common ocular conditions.6-8 Patients with DED can have chronic disease with episodic flares in which symptoms worsen for a short period of time.9 In fact, most patients with DED experience short-term episodic flares instead of continuous symptoms.10,11 Dry eye symptoms, whether they’re chronic or episodic, cause ocular discomfort and pain which can have a significant impact on an individual’s quality of life by interfering with their ability to see and perform daily activities, such as work.9,12 Reduced work productivity can have a substantial economic impact.12,13 One study (N=2171 DED respondents) found the estimated average combined direct and indirect cost of managing DED to be around 55 billion dollars annually in the US.13

More than an estimated 16 million adults have been diagnosed with DED in the United States.6

Artificial tears are a mainstay for treating DED and while they provide relief, they do not contain the same components as natural tears or treat the underlying causes of DED.14,15 Prescription medications for chronic DED are often limited by the length of time required for benefits to become apparent to the affected individual, they sometimes take weeks to months to exert modest effects.15-17 These medications are often poorly tolerated and many contain preservatives that may contribute to ocular discomfort.18-20 Drawbacks such as these may be reasons why patient describe experiencing product dissatisfaction, low adherence to a treatment regimen, and the high discontinuation of use rates that are often associated with these treatment options.21
Currently there are FDA-approved prescription medications available for DED.22 However, there are opportunities for novel approaches to the chronic treatment of DED and short-term treatment of episodic DED that could have a rapid onset, improved product tolerability, a longer durability of effect and improved patient compliance.

About Allergic Conjunctivitis
Allergic conjunctivitis (AC) is allergen-induced inflammation of the conjunctiva – a thin, clear membrane covering the front surface of the eye.23 It has been estimated to affect up to 40% of the general population in the US, yet it remains underreported.24,25 AC represents a growing problem in the US with the prevalence of AC-associated nasal and ocular symptoms more than doubling over the past 20 years.26 Like other OSDs, AC-related ocular itching and redness can be bothersome and burden patients by adversely affecting their sleep and daily activities.27,28 Ocular allergy symptoms are also associated with decreased work productivity represented by impairment while working and an increase in hours of work missed.27

Management of AC symptoms often begins with patients treating themselves using over-the-counter medications.25 Although effective for mild symptoms, these medications may be inadequate for moderate to severe AC symptoms.29 If symptoms are not adequately controlled, prescription eye drops may be added to the regimen.29 Most eye drops for treating AC require multiple daily instillations which may lead to either poor treatment adherence or treatment discontinuation.30
Learn more…
about how Ocular Therapeutix is addressing the challenges of treatments for allergic conjunctivitis.
REFERENCES: 1. Gipson IK. Invest Ophthalmol Vis Sci. 2007;48(10):4390-4398. 2.Scott CA, et al. American Optometric Association. Care of the Patient with Ocular Surface Disorders. Updated December, 2010. Accessed December 20, 2022. https://bit.ly/3SAUpA5. 3. Leung EW, et al. J Glaucoma. 2008;17(5):350-355. 4. Leonardi A, et al. Ocul Immunol Inflamm. 2021;29(6):1168-1176. 5. Craig JP, et al. Ocul Surf. 2017;15(3):276-283. 6. Farrand KF, et al. Am J Ophthalmol. 2017;182:90-98. 7. Stapleton F, et al. Ocul Surf. 2017;15(3):334-365. 8. Papas EB. Ophthalmic Physiol Opt. 2021;41(6):1254-1266. 9. Gupta PK, et al. Ther Adv Ophthalmol. 2021;13:25158414211012797. 10. Perez VL, et al. Exp Eye Res. 2020;201:108294. 11. Starr CE, et al. Ocul Surf. 2021;22:51-59. 12. Uchino M, et al. Curr Ophthalmol Rep. 2013;1(2):51-57. 13. Yu J, et al. Cornea. 2011;30(4):379-387. 14. Kim M, et al. BMJ Open Ophthalmol. 2021;6(1):e000697. 15. Trattler W, et al. Clin Ther. 2006;28(11):1848-1856. 16. Xiidra® [package insert]. Lexington, MA: Shire US Inc.; 2016 17. Tyrvaya® [package insert]. Princeton, NJ: Oyster Point Pharma, Inc.; 2021. 18. White DE, et al. Clin Ophthalmol. 2020;14:875-883. 19. Eysuvis® [package insert]. Watertown, MA: Kala Pharmaceuticals; 2020. 20. Nasser L, et al. Clin Ophthalmol. 2018;12:1519-1525 21. White DE, et al. Clin Ophthalmol. 2019;13:2285-2292. 22. Mukamal R. American Academy of Ophthalmology. Improved Dry Eye Drugs for 2022 and Beyond. Published November 4, 2021. Accessed December 20, 2022. https://www.aao.org/eye-health/tips-prevention/new-dry-eye-treatments-ocular-surface-disease. 23. Dupuis P, et al. Allergy Asthma Clin Immunol. 2020;16:5. 24. Singh K, et al. J Allergy Clin Immunol. 2010;126(4):778-783.e6. 25. Bielory L, et al. Ann Allergy Asthma Immunol. 2020;124(2):118-134. 26. Meng Q, et al. Ann Allergy Asthma Immunol. 2016;116(2):118-125.e5. 27. Virchow JC, et al. J Med Econ. 2011;14(3):305-314. 28. Maspero J, et al. Clin Exp Allergy. 2012;42(12):1684-1696. 29. Varu DM, et al. Ophthalmology. 2019;126(1):P94-P169. 30. Carr W, et al. Allergy Rhinol (Providence). 2016;7(2):107-114.