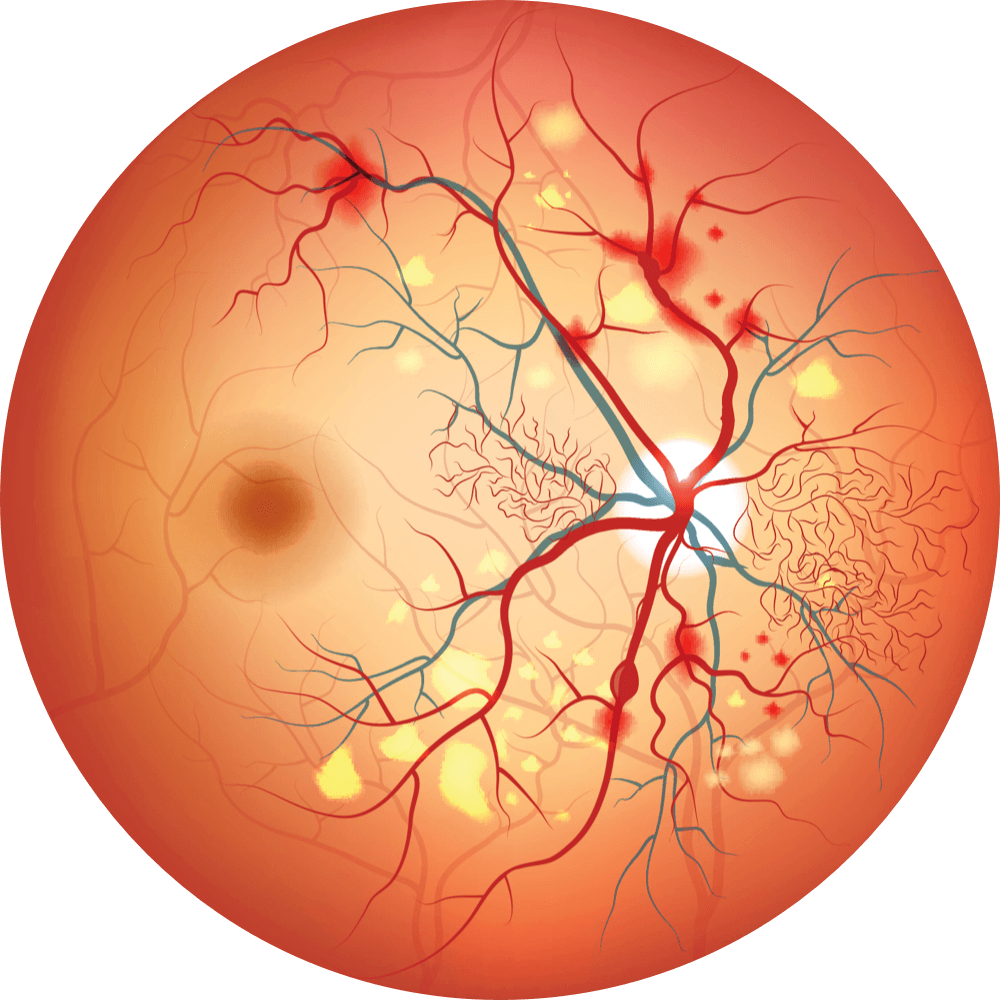
Retinal Diseases
Retinal diseases constitute a group of conditions that affect the retina – a thin layer of tissue that lines the back of the eye. The retina contains millions of light-sensitive rods, cones, and other nerve cells that are responsible for receiving and organizing visual information.1 An estimated 401.6 million people around the world suffer from some form of retinal disease.2 Many of these diseases and conditions can lead to vision loss or serious visual impairment, limiting sharpness of vision and leading to significant impact on an individual’s quality of life.3, 7-9 Age-related macular degeneration and diabetic eye diseases are the most common diseases of the retina accounting for 42.4% of all cases of retinal disease in the US.4 They are the leading causes of vision loss or blindness and are becoming more important because of aging populations and the increasing incidence of diabetes.5-8
About Age-related Macular Degeneration (AMD)
AMD is the leading cause of vision loss and blindness in the older US population.5 The projected number of people with AMD in 2020 globally was 196 million and is estimated to increase to 288 million by 2040.9 Stated another way, AMD affects one in eight people 60 years of age or older in developed countries and is the most common cause of irreversible blindness in this age group.10 In the United States, the estimated number of people with AMD is expected to double from 9 million to 18 million by 2050 since longer life expectancy is likely to lead to further increases in the number of individuals with AMD.7,11
The projected number of people with AMD in 2020 globally was 196 million.9


AMD is often grouped into two basic clinical categories: the ‘dry’ atrophic form and the exudative neovascular, or ‘wet’ form.12 While wet AMD affects only 10-15% of patients with AMD, it accounts for more severe AMD-related vision loss compared to dry AMD.12 Without prompt and continuous treatment to control exudative activity, patients may develop irreversible vision loss; however, with proper treatment, patients may maintain visual function for a period of time and may temporarily regain vision they might have previously lost.13-15 Not surprisingly, irreversible eye diseases such as wet AMD have a considerable detrimental impact on overall patient quality of life, such as loss of reading and driving.16,17

About Diabetic Retinopathy (DR)
DR is a leading cause of visual loss in the working-age population.6,8 Globally, the number of people living with DR in 2010 was estimated to be 126.6 million and is expected to increase to 191 million by 2030.18 Because DR affects approximately 35% to 49% of diabetes patients, this increasing trend is likely driven by the expanding diabetes epidemic worldwide.8,19 In the United States, DR affected nearly 8 million people in 2020 and the number is expected to double by 2050.20
The progression of DR from non-proliferative stages (NPDR) to proliferative stages (PDR) can cause life-limiting vision loss and blindness.21,22 To add to this disease concern, diabetic macular edema (DME) can occur at any stage of DR and represents the most common cause of vision loss in patients with DR.21 Consequently, DR and associated visual impairment can limit patients’ day-to-day tasks and, importantly, diabetes management activities.23 Patients with DR have reported reduced physical, emotional and social well-being.8 It is estimated that health-related quality of life may be reduced by up to half in DR compared to diabetic patients without DR.8 Needless to say, the impact of DR on patients’ lives is substantial.

Challenges with Treatments for wet AMD and DR
Although anti-vascular endothelial growth factor therapy (VEGF) therapy can minimize vision loss in wet AMD and DR patients, real-world data suggest frequent intravitreal injections create a high treatment burden for patients, caregivers and providers.8,24,25 There is a physical and psychological burden for patients and substantial time burden on caregivers.26-28 AMD patients report monthly intravitreal injections are moderately stressful to go through and that they are fearful of the side effects of intravitreal injections.26,29 Anti-VEGF agents are also associated with a substantial financial burden for patients and the healthcare system, due to their high cost and the need for frequently repeated treatments plus clinic visits.30 These factors may lead to reduced compliance to anti-VEGF therapy. In one real world study of approximately 9000 wet AMD patients, approximately 20% of patients were lost to follow-up within 12 months after initiating anti-VEGF injections.31 Additionally, 20-40% of wet AMD patients and 15-20% of DR patients do not adequately respond to anti-VEGF therapy or experience a slow loss of efficacy after repeated administration and may require alternate management strategies.32,33 An effective, durable, long-acting treatment that substantially reduces the injection burden on wet AMD and DR patients may improve compliance to a patient’s prescribed therapy and potentially either slow or halt disease-related vision loss.
REFERENCES: 1. Masland RH. Neuron. 2012;76(2):266-280. 2. Market Scope. 2022 Retinal Pharmaceuticals Market Report: Global Analysis for 2021 to 2027. Published August 2022. 3. Prem Senthil M, et al. J Patient Rep Outcomes. 2017;1(1):15. 4. Rosenblatt TR, et al. Ophthalmic Surg Lasers Imaging Retina. 2021;52(1):29-36. 5. Centers for Disease Control and Prevention. Learn About Age-Related Macular Degeneration. Updated November 23, 2020. Accessed December 7, 2022. http://bit.ly/41sECrc. 6. Wang W, et al. Int J Mol Sci. 2018;19(6):1816. 7. Di Carlo E, et al. J Clin Med. 2021;10(15):3297. 8. Wong TY, et al. Nat Rev Dis Primers. 2016;2:16012. 9. Wong WL, et al. Lancet Glob Health. 2014;2(2):e106-e116. 10. Vyawahare H, et al. Cureus. 2022;14(9):e29583. 11. Rein DB, et al. Arch Ophthalmol. 2009;127(4):533-540. 12. Gehrs KM, et al. Ann Med. 2006;38(7):450-471. 13. Flaxel CJ, et al. Ophthalmology. 2020;127(1):P1-P65. 14. Fleckenstein M, et al. Nat Rev Dis Primers. 2021;7(1):31. 15. Maguire MG, et al. Ophthalmology. 2016;123(8):1751-1761. 16. Gupta P, et al. Sci Rep. 2022;12(1):8465. 17. Taylor DJ, et al. BMJ Open. 2016;6(12):e011504. 18. Zheng Y, et al. Indian J Ophthalmol. 2012;60(5):428-431. 19. Arup Das. Invest. Ophthalmol. Vis. Sci. 2016;57(15):6669-6682. 20. The American Society of Retina Specialists. Americans in the dark on diabetic retinopathysymptoms, risks, survey finds. Accessed December 8, 2022. https://www.asrs.org/sections/member-news/5097/Americans-in-the-Dark-on-Diabetic-Retinopathy-Symptoms-Risks-Survey-Finds. 21. Duh EJ, et al. JCI Insight. 2017;2(14):e93751. 22. Morello CM. Am J Health Syst Pharm. 2007;64(17 Suppl 12):S3-S7. 23. Coyne KS, et al. Fam Pract. 2004;21(4):447-453. 24. Okada M, et al. JAMA Ophthalmol. 2021;139(7):769-776 [erratum in: 2022;140(6):653] 25. Gale RP, et al. Acta Ophthalmol. 2023;101(1):e26-e42. 26. Gualino V, et al. J Fr Ophtalmol. 2020;43:1047-1053. 27. Thier A, et al. Disabil Rehabil. 2022;44(5):661-671. 28. Prenner JL, et al. Am J Ophthalmol. 2015;160(4):725-31.e1. 29. Senra H, et al. Graefes Arch Clin Exp Ophthalmol. 2016;254(10):1873-1880. 30. ElSheikh RH, et al. Biomolecules. 2022;12:1629. 31. Obeid A, et al. JAMA Ophthalmol. 2018;136:1251-1259. 32. Wallsh JO, et al. Cells. 2021;10:1049. 33. Ricci F, et al. Int J Mol Sci. 2020;21:8242.